ADHD Evaluations: Examining Impairments Beyond Symptomology
Attention-Deficit/Hyperactivity Disorder (ADHD) is a neurodevelopmental disorder marked by symptoms of inattention and/or hyperactivity and impulsivity that interfere with functioning and development. Both the outlined criteria in the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition, Text Revision (DSM-5-TR; APA, 2022) and the determination of educational eligibility under the Individuals with Disabilities Education Improvement Act (IDEA; 2004) require that reported problems be associated with clinically significant impairment in the youth’s functioning in various domains including social, academic, and occupational contexts.
Impairment associated with ADHD can manifest in multiple ways, such as greater risk for suspension, expulsion, school dropout, substance use, difficulties at school or in personal relationships, or mental health problems that continue or develop through adulthood1.
Why is it important to examine symptoms and impairments in ADHD evaluations?
Examining symptoms and impairment are a critical part of ADHD evaluation; although they are often related concerns, each area provides distinct information2,3. For example, a study found that symptoms reported were not enough to capture the full impact of treatment4. Information on functional impairment was needed to understand continued problems experienced and how to direct additional support for the youth. Additionally, research has found that adding impairment data to symptom-based diagnoses reduced the number of ADHD diagnoses made by as much as 77%, which may help address common concerns about overdiagnosis of ADHD in youth5. Identifying clinically significant levels of impairment is a critical component of a standardized and comprehensive diagnosis of ADHD.
How can we measure impairment?
Given the research about the importance of impairment as part of the whole picture of an ADHD diagnosis, the recently published Conners 4th Edition™ (Conners 4®; Conners, 2022) now includes a set of scales devoted to measuring these potential concerns. In addition to the Content Scales that evaluate key features related to ADHD and the DSM Symptom Scales that map directly onto the symptom criteria for ADHD, the Conners 4 Impairment & Functional Outcome Scales provide indications specifically about problems in functioning outcomes that are commonly reported with the symptoms of ADHD. The Impairment & Functional Outcome Scales cover three important domains: Schoolwork, Peer Interaction, and Family Life. They are available across all raters (i.e., Parent, Teacher, and youth Self-Report) to better inform diagnosis and treatment planning (note that Family Life is only applicable for Parent and Self-Report forms).
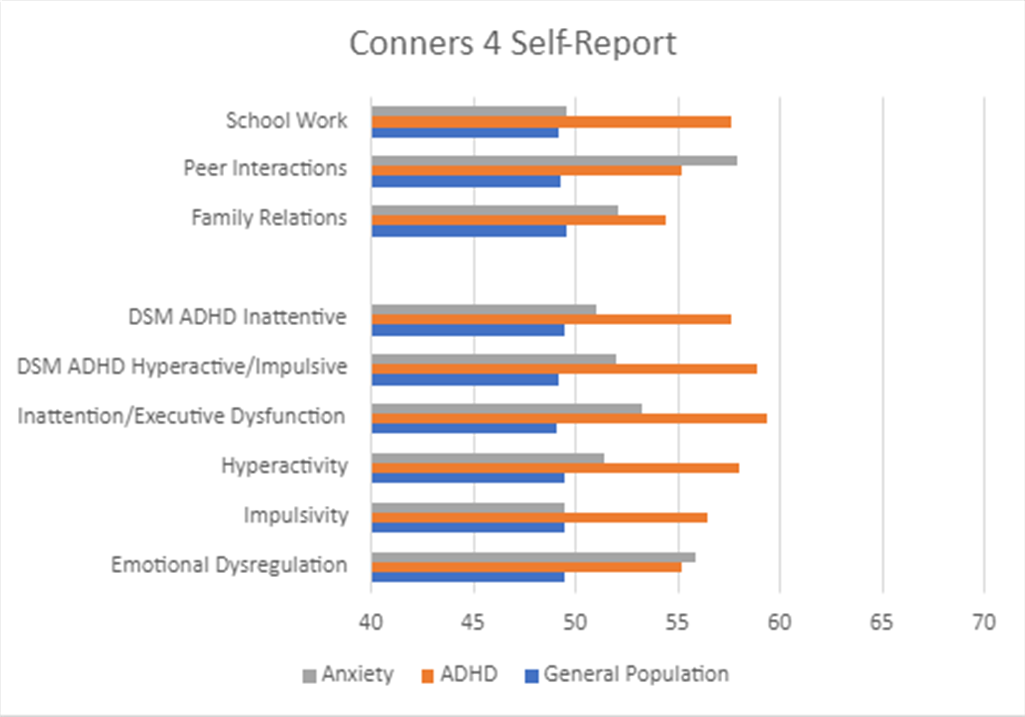
The development of the Conners 4 Impairment & Functional Outcome Scales involved thorough validation and research. Data were collected from youth with and without clinical disorders, and their scores were compared across groups (i.e., undiagnosed youth vs. youth with an ADHD diagnosis vs. youth with a diagnosis of an anxiety disorder, including Generalized Anxiety, Social Anxiety, Separation Anxiety, and Panic Disorder). The results of these studies are summarized in the graphs below. Figure 1 displays average scores from Parent ratings of youth with ADHD, anxiety, or no diagnosis; Figure 2 presents differences between groups for Teacher ratings, and Figure 3 presents differences between groups from youth Self-Report .
Figure 1. Group Differences: Conners 4 Parent
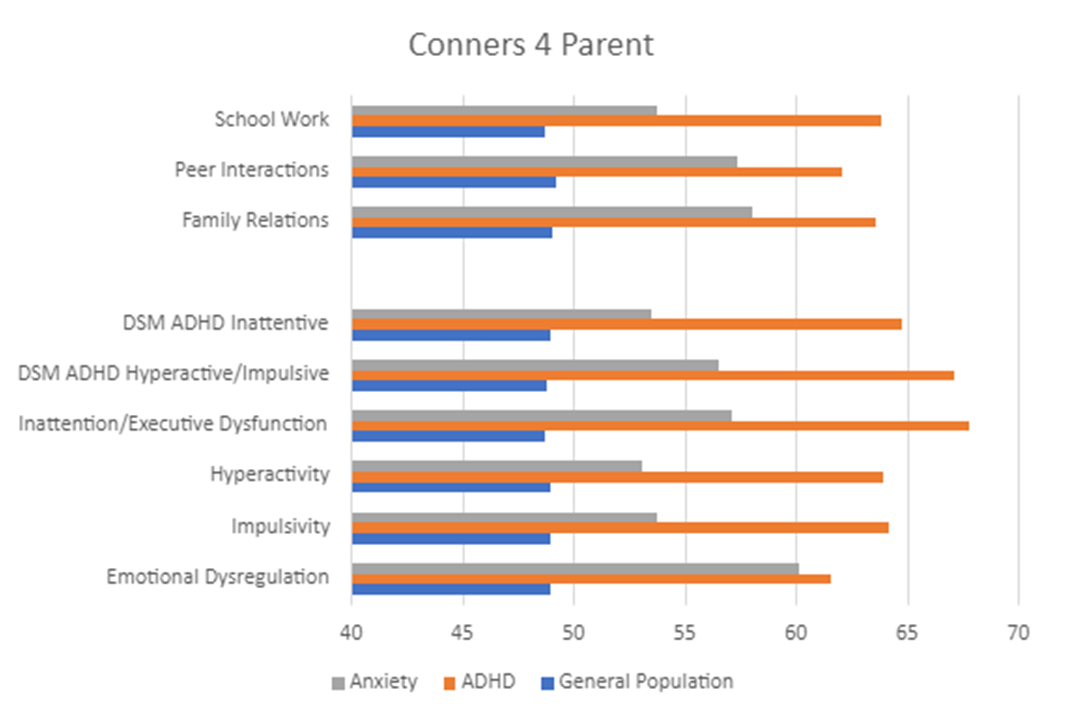
Figure 2. Group Differences: Conners 4 Teacher
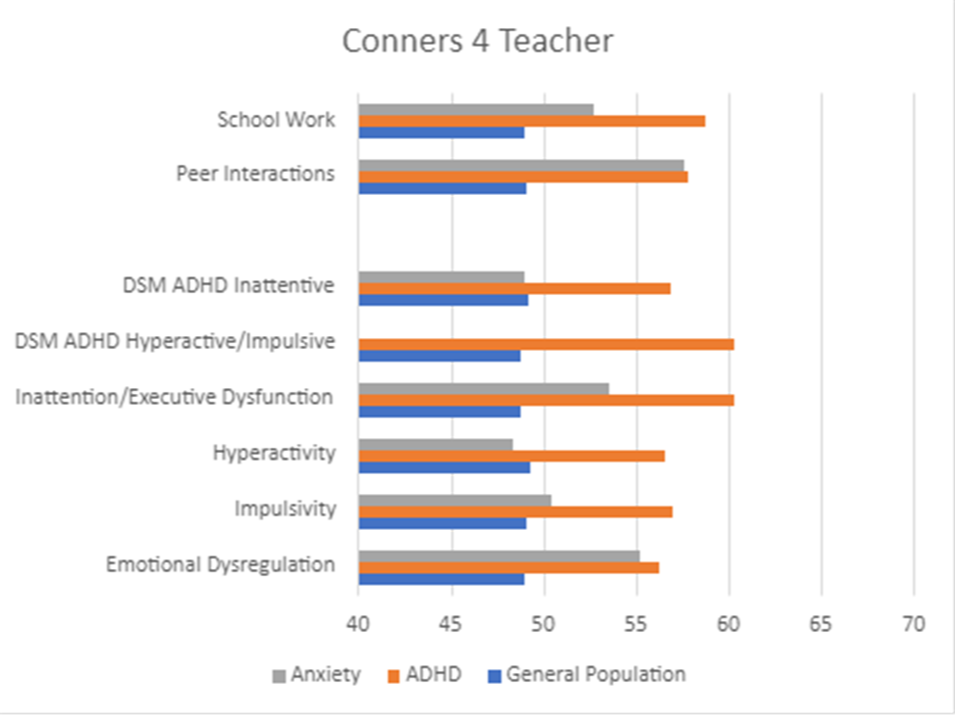
Figure 3. Group Differences: Conners 4 Self-Report
How does impairment differ between youth with different diagnoses?
Across all raters, the clinical groups (i.e., youth with ADHD or anxiety) displayed higher scores for reported impairment than the general population group. The scores for the Impairment & Functional Outcome Scales (Schoolwork, Peer Relations, Family Life) follow very similar patterns as the Content and DSM Symptom Scales. That is, youth without a clinical diagnosis typically had low scores (below 50) for all of the scales. However, youth with a clinical diagnosis typically had elevated scores for scales that measured symptoms and for scales that measure functional impairment.
Youth with ADHD consistently displayed the highest scores for all scales across all raters, which was expected given that the Conners 4 was developed specifically to address symptoms and features common to ADHD. Youth with anxiety in this study did not have a co-occurring diagnosis of ADHD; however, their scores are still slightly elevated on many of the scales, as some of the symptoms and features are transdiagnostic and will also appear for youth with other clinical disorders. In particular, youth with anxiety may experience significant challenges with Emotional Dysregulation, as seen in our results, where this group’s scores are nearly as high as the ADHD group (see Figure 1).
The trend of these results is consistent with past research. Youth with ADHD score higher than youth with anxiety, who in turn, score higher than youth without a diagnosis. These results help demonstrate the accuracy with which the Conners 4 can measure symptoms and impairments.
Symptoms alone are not enough to understand how a youth functions or how they can best be supported. Functional impairment is a necessary consideration that should be involved in all clinical evaluations of ADHD, along with other disorders, as many of the same concerns are not solely unique to youth with ADHD. Assessing functional impairment is part of the diagnostic requirement for ADHD, as stated in the DSM-5-TR and IDEA.
To summarize, information on impairment across various domains is valuable because they provide additional insight into what the youth are experiencing in their day-to-day functioning. It provides a more comprehensive profile of problems and risks and is critical for the diagnosis and treatment planning of ADHD.
Learn more about MHS’ Conners 4.
For further reading on ADHD, check out the following blogs:
The importance of Multi-Rater Assessments in ADHD evaluation
The link between sleep problems and ADHD
The critical need to address self-harm during youth ADHD assessment
1 Watabe, Y., Owens, J. S., Evans, S. W., & Brandt, N. E. (2014). The relationship between sluggish
cognitive tempo and impairment in children with and without ADHD. Journal of Abnormal Child Psychology, 42, 105-115.
2 Gathje, R. A., Lewandowski, L. J., & Gordon, M. (2008). The role of impairment in the diagnosis of
ADHD. Journal of Attention Disorders, 11(5), 529-537
3 Johnstone, J. M., Leung, B. M., Srikanth, P., Hatsu, I., Perez, L., Gracious, B., … & Arnold, L. E. (2020).
Development of a composite primary outcome score for children with attention-deficit/hyperactivity disorder and emotional dysregulation. Journal of Child and Adolescent Psychopharmacology, 30(3), 166-172.
4 Coghill, D. R., Banaschewski, T., Soutullo, C., Cottingham, M. G., & Zuddas, A. (2017). Systematic review
of quality of life and functional outcomes in randomized placebo-controlled studies of medications for attention-deficit/hyperactivity disorder. European Child & Adolescent Psychiatry, 26, 1283-1307.
5 Gordon, M., Antshel, K., Faraone, S., Barkley, R., Lewandowski, L., Hudziak, J. J., … & Cunningham, C.
(2006). Symptoms versus impairment: The case for respecting DSM-IV’s Criterion D. Journal of Attention Disorders, 9(3), 465-475.










